Chest pain has a way of stopping time. One moment you’re going about your day, the next you’re frozen—hand on your chest, heart racing, mind spiraling. Is this serious? Am I overreacting? Should I wait it out, call my doctor, or call 911?
This question sends millions of people to search engines and emergency rooms every year. And for good reason. Chest pain can range from completely harmless to immediately life-threatening, and telling the difference on your own isn’t always possible.
This article will walk you through when chest pain is an emergency, what symptoms should never be ignored, how doctors think about chest pain, and when it may be safe to seek non-emergency care. The goal is not to make you anxious—but to give you clarity, confidence, and the ability to act quickly when it matters most.
Chest Pain Isn’t Always “Pain” — and That Matters
One of the most dangerous misconceptions about heart and chest emergencies is the idea that they always involve dramatic, crushing pain in the center of the chest.
In medicine, clinicians often talk about “chest pain equivalents.” These are symptoms that signal possible heart or lung emergencies even if no classic pain is present. Chest discomfort may feel like pressure, tightness, heaviness, squeezing, fullness, or burning. It may show up in places you wouldn’t expect—such as the jaw, neck, shoulder, arm, upper back, or even the upper abdomen.
Shortness of breath, unexplained fatigue, nausea, lightheadedness, or breaking out in a cold sweat can also be warning signs. In some cases, especially in women and older adults, these symptoms appear without any chest pain at all.
This is why healthcare organizations like American Heart Association and American College of Cardiology emphasize that chest pain and its equivalents should be taken seriously and evaluated promptly.
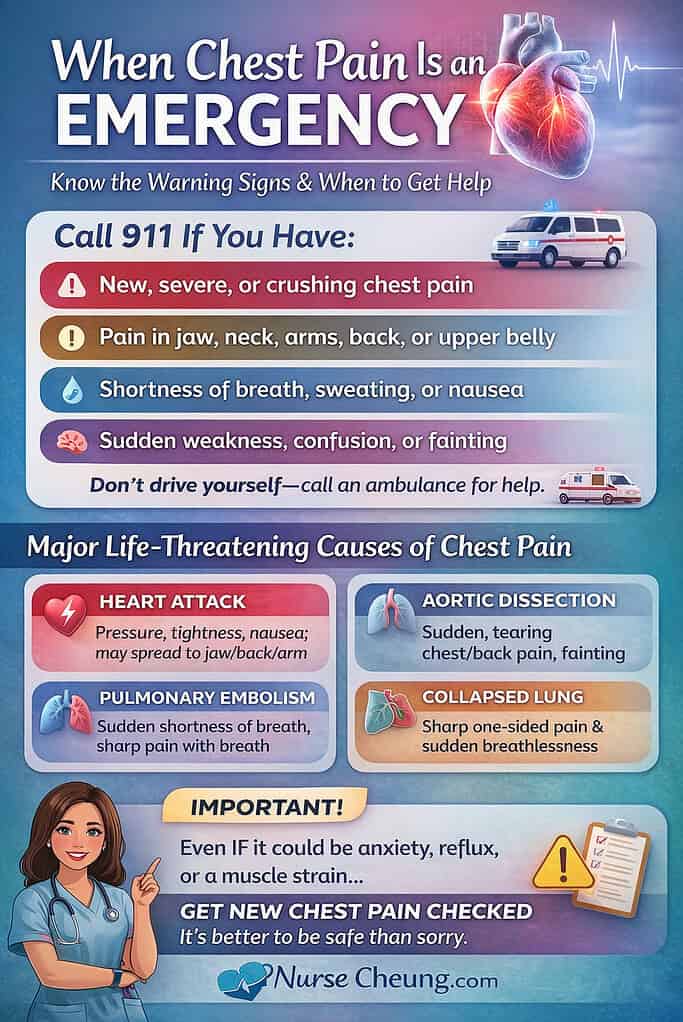
The Non-Negotiable Red Flags: When to Call 911 Immediately
There are moments when waiting, Googling, or “seeing if it passes” can be dangerous. You should seek emergency care right away if chest pain or chest-related symptoms are:
New, severe, crushing, or pressure-like
Lasting more than a few minutes, or coming and going repeatedly
Occurring with shortness of breath
Accompanied by sweating, nausea, vomiting, dizziness, or fainting
Spreading to the arm, shoulder, jaw, neck, or back
Associated with sudden weakness, confusion, trouble speaking, or vision changes
Occurring after cocaine or stimulant use
Happening in someone with known heart disease, prior heart attack, or multiple cardiovascular risk factors
If you are unsure whether your symptoms are serious, that uncertainty alone is reason enough to seek emergency care. Medical guidelines consistently advise that people with acute chest symptoms should call 911 rather than drive themselves, because emergency medical services can begin evaluation and treatment immediately.
The Most Dangerous Causes of Chest Pain
Not all chest pain is life-threatening—but some causes are extremely time-sensitive. These are the conditions emergency clinicians are trained to rule out first.
Heart Attack (Acute Coronary Syndrome)
A heart attack occurs when blood flow to part of the heart muscle is blocked. While chest pressure or heaviness is common, symptoms can be surprisingly subtle.
People may experience discomfort that feels like indigestion, tightness, or burning rather than sharp pain. Shortness of breath, nausea, sweating, and pain radiating to the jaw or arm are classic warning signs. Women are more likely than men to report fatigue, nausea, or back and shoulder pain instead of dramatic chest pressure.
Prompt treatment saves heart muscle—and lives. That’s why emergency departments prioritize rapid testing, including an electrocardiogram and blood tests such as high-sensitivity troponin, to identify heart damage as early as possible.
Aortic Dissection
An aortic dissection is a tear in the inner layer of the body’s largest artery. It is less common than heart attack, but often far more deadly.
People frequently describe the pain as sudden, severe, and unlike anything they have felt before. It may feel ripping or tearing and often radiates to the upper back. Fainting, stroke-like symptoms, or shock can occur.
Time is critical. Mortality increases rapidly without immediate surgical care, which is why sudden severe chest or back pain should never be ignored.
Pulmonary Embolism
A pulmonary embolism occurs when a blood clot blocks blood flow in the lungs. Symptoms often include sudden shortness of breath, sharp chest pain that worsens with deep breathing, rapid heart rate, coughing, or fainting.
Risk factors include recent surgery, prolonged immobility, pregnancy or postpartum status, hormone therapy, cancer, and prior blood clots. According to Centers for Disease Control and Prevention, pulmonary embolism is a medical emergency that requires immediate treatment.
Pneumothorax (Collapsed Lung)
A pneumothorax happens when air leaks into the space between the lung and chest wall, causing the lung to collapse. It can occur spontaneously or after trauma.
Symptoms typically include sudden chest pain and shortness of breath, often on one side. Some cases are mild, but others can become life-threatening without urgent care.
Esophageal Rupture (Boerhaave Syndrome)
Although rare, an esophageal rupture is one of the most dangerous causes of chest pain. It often occurs after forceful vomiting or severe retching.
People experience sudden, severe chest pain and rapidly become very ill. Mortality rates are high, especially when diagnosis is delayed, making this a true surgical emergency.
Chest Pain That Is Usually Not Life-Threatening
Many people evaluated for chest pain do not end up having a heart or lung emergency. Common non-life-threatening causes include:
Costochondritis, an inflammation of the cartilage connecting the ribs to the breastbone
Gastroesophageal reflux disease (GERD) or esophageal spasm
Muscle strain from physical activity or coughing
Anxiety or panic attacks
Pericarditis, inflammation of the lining around the heart
While these conditions are generally less dangerous, the key point is this: they are diagnoses made after serious causes are ruled out. New or unexplained chest pain should not be self-diagnosed, even if it feels familiar.
What Happens When You Go to the ER for Chest Pain
Fear of the emergency room keeps many people from seeking care. Understanding what actually happens can ease that anxiety.
When you arrive, clinicians focus on ruling out life-threatening conditions quickly. You can expect vital signs, an electrocardiogram, blood tests, and sometimes imaging such as a chest X-ray or CT scan. These tests help doctors determine whether your heart, lungs, or major blood vessels are involved.
Importantly, being “cleared” does not mean your symptoms were imaginary. It means dangerous causes were ruled out—and that reassurance has real value.
When Urgent Care or Your Doctor May Be Appropriate
There are situations where chest discomfort may be safely evaluated outside the emergency department. This typically includes mild, familiar symptoms that have been previously evaluated and diagnosed, especially when no red flags are present.
However, urgent care is not equipped to rule out heart attacks, pulmonary embolisms, or aortic dissections. If there is any doubt, emergency care is the safer choice.
A Simple Rule for Deciding in the Moment
When chest symptoms appear, ask yourself:
Is this new or unexplained?
Is this stopping me from normal activity?
Would I feel unsafe being alone with these symptoms?
If the answer to any of these questions is yes, emergency evaluation is the right decision.
Conclusion: When in Doubt, Choose Safety
Chest pain sits at the intersection of fear and uncertainty—and for good reason. Some causes are minor and treatable, while others are silent, fast-moving, and deadly.
The most important takeaway is this: you are never wrong for seeking help when it comes to chest pain. Acting early is not panic. It is prevention.
Trust your instincts. Listen to your body. And remember that emergency care exists not just to save lives, but to provide clarity, reassurance, and peace of mind when it matters most.
If this article helped you better understand when chest pain is an emergency, consider sharing it with someone you care about. Clear information saves lives—and knowledge is most powerful when it’s shared.