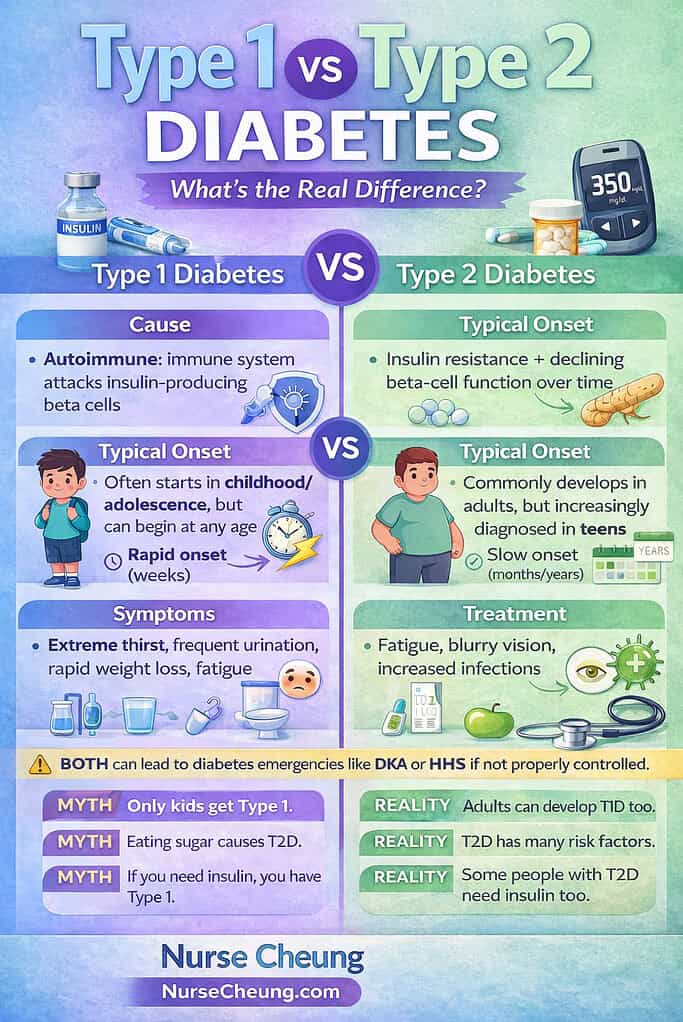
Two people can both say, “I have diabetes,” and yet be dealing with conditions that are biologically, clinically, and emotionally very different.
That confusion is not just academic—it shapes how people are treated, how quickly they get help, and how much stigma they carry. Type 1 and Type 2 diabetes share a name, but they are not interchangeable diagnoses, and assuming they are can lead to dangerous misunderstandings.
This article breaks down Type 1 vs Type 2 diabetes in clear, practical terms. We’ll explore what causes each type, how they show up in real life, how they’re treated, and why the difference truly matters—for patients, families, and anyone trying to understand diabetes beyond stereotypes.
What Is Diabetes, Really?
At its core, diabetes is a problem with blood glucose regulation.
Glucose is the body’s primary source of energy. To move glucose from the bloodstream into cells, the body relies on a hormone called insulin, produced by the pancreas. When insulin is missing, ineffective, or both, glucose builds up in the blood instead of being used for fuel. Over time, elevated blood sugar damages blood vessels, nerves, kidneys, eyes, and the heart.
All forms of diabetes involve this imbalance—but how and why it happens is what separates Type 1 from Type 2.
Type 1 Diabetes: When the Immune System Turns on Itself
Type 1 diabetes is an autoimmune disease.
In this condition, the immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. As a result, the body produces little to no insulin. Without external insulin, survival is not possible.
Key characteristics of Type 1 diabetes
Caused by an autoimmune response
Leads to absolute insulin deficiency
Requires lifelong insulin therapy
Not preventable and not caused by lifestyle
Type 1 diabetes often develops quickly. Symptoms can appear over weeks or even days and may include:
Excessive thirst
Frequent urination
Unexplained weight loss
Extreme fatigue
Blurred vision
Because insulin levels drop sharply, people with Type 1 diabetes are at high risk for diabetic ketoacidosis (DKA), a life-threatening emergency caused by insulin deficiency.
A critical misconception is that Type 1 diabetes only affects children. While it is commonly diagnosed in youth, adults can and do develop Type 1 diabetes, sometimes later in life and sometimes misdiagnosed at first.
Clinical guidelines and classifications from the American Diabetes Association make it clear: age does not define the diagnosis—biology does.
Type 2 Diabetes: Insulin Resistance and Metabolic Burnout
Type 2 diabetes is primarily a metabolic condition characterized by insulin resistance.
In the early stages, the pancreas still produces insulin, sometimes in large amounts. The problem is that the body’s cells—particularly in muscle, fat, and liver tissue—don’t respond to insulin effectively. To compensate, the pancreas works overtime. Eventually, it can no longer keep up, and blood glucose levels rise.
Key characteristics of Type 2 diabetes
Driven by insulin resistance and progressive beta-cell dysfunction
Develops gradually over time
Strongly influenced by genetics, physiology, and environment
Often manageable initially without insulin
Type 2 diabetes may remain silent for years. Many people are diagnosed during routine blood work or after complications begin to appear. When symptoms do occur, they can include:
Fatigue
Blurred vision
Slow-healing wounds
Increased infections
Tingling or numbness in hands and feet
Contrary to popular belief, Type 2 diabetes is not simply caused by sugar intake. Genetics, hormonal signaling, body composition, inflammation, sleep, stress, and socioeconomic factors all play roles. Simplifying it to “poor choices” ignores the complex biology involved—and fuels stigma.
Type 1 vs Type 2 Diabetes at a Glance
Although both conditions result in high blood sugar, they differ in important ways:
Type 1 diabetes involves autoimmune destruction of insulin-producing cells and requires insulin from diagnosis onward. Type 2 diabetes involves insulin resistance, develops gradually, and may initially be managed with lifestyle changes and medications.
People with Type 1 diabetes are more prone to rapid metabolic emergencies like DKA, while people with Type 2 diabetes are more likely to experience long-term complications if the condition goes undetected or untreated.
Understanding these distinctions is not optional—it directly affects safety and outcomes.
How Diabetes Is Diagnosed and Why Type Matters
Diabetes is diagnosed using standardized blood tests such as:
Hemoglobin A1C
Fasting plasma glucose
Oral glucose tolerance testing
Random plasma glucose with symptoms
These tests confirm the presence of diabetes, but they do not always determine the type on their own.
In many cases—especially in adults—Type 1 diabetes, Type 2 diabetes, and other forms can overlap in appearance at diagnosis. Misclassification can delay appropriate treatment, increasing the risk of complications.
Public health data from the Centers for Disease Control and Prevention shows that a significant number of adults with diabetes are initially diagnosed without clear subtype differentiation, highlighting the importance of follow-up evaluation.
The Gray Area: LADA and “Type 1.5” Diabetes
Some adults are diagnosed with Type 2 diabetes, respond briefly to oral medications, and then rapidly lose glucose control. In many of these cases, the underlying condition is LADA (Latent Autoimmune Diabetes in Adults).
LADA is an autoimmune form of diabetes that develops more slowly than classic childhood-onset Type 1 diabetes. Because insulin dependence isn’t immediate, it’s often mistaken for Type 2 diabetes early on.
This gray area reinforces an essential truth: diabetes exists on a spectrum, and labels must serve patients—not convenience.
Diabetes Emergencies: DKA vs HHS
One of the most important practical differences between Type 1 and Type 2 diabetes lies in acute emergencies.
Diabetic Ketoacidosis (DKA)
DKA occurs when the body lacks insulin and begins breaking down fat for energy, producing ketones that acidify the blood. It is most common in Type 1 diabetes but can occur in Type 2 under severe stress.
Symptoms include:
Nausea and vomiting
Abdominal pain
Rapid, deep breathing
Fruity-smelling breath
Confusion or altered mental status
Hyperglycemic Hyperosmolar State (HHS)
HHS is more commonly associated with Type 2 diabetes and involves extreme hyperglycemia and dehydration without significant ketosis. It develops more slowly but can be equally life-threatening.
Both conditions require immediate medical care.
Clinical emergency guidance from agencies such as the National Institute of Diabetes and Digestive and Kidney Diseases emphasizes early recognition and prompt treatment as lifesaving.
Can Type 2 Diabetes Be Reversed?
This is one of the most common—and most misunderstood—questions about diabetes.
The correct medical term is remission, not cure.
Some individuals with Type 2 diabetes can achieve sustained normal blood glucose levels without glucose-lowering medications, particularly after significant weight loss or metabolic interventions. However, this does not mean the underlying susceptibility disappears.
Remission requires ongoing monitoring and lifestyle maintenance. Relapse is possible, especially if the factors that contributed to insulin resistance return.
Major professional organizations, including the American Diabetes Association, define remission carefully to avoid misleading claims and false expectations.
New Developments in Diabetes Care
Diabetes treatment has evolved dramatically in recent years.
For Type 1 diabetes, immune-modifying therapies have been developed to delay disease onset in high-risk individuals. One such therapy has received regulatory approval from the Food and Drug Administration, marking a milestone in preventive care.
For Type 2 diabetes, newer medication classes not only lower blood sugar but also protect the heart and kidneys—two organs disproportionately affected by diabetes complications.
Technology has also transformed daily management. Continuous glucose monitors and smart insulin delivery systems have improved safety, precision, and quality of life for millions of people.
The Myths That Still Do Harm
Despite decades of research, several myths persist:
Type 1 diabetes is not caused by sugar or parenting choices
Type 2 diabetes is not a personal failure
Insulin use does not mean someone “gave up”
Thin people can have Type 2 diabetes, and larger bodies can have Type 1
Misinformation fuels stigma, delays diagnosis, and discourages people from seeking care. Correcting these myths is not just educational—it’s ethical.
Same Name, Different Realities
Type 1 and Type 2 diabetes may share a name, but they represent distinct biological pathways, different risks, and unique treatment needs.
Understanding the real difference moves the conversation away from blame and toward biology, evidence, and compassion. It empowers patients to advocate for proper care and helps families, educators, and healthcare professionals respond appropriately.
Diabetes is common—but misunderstanding it doesn’t have to be.
The more accurately we talk about it, the safer and more supported people living with diabetes will be.
If this article clarified something you’ve wondered about—or corrected something you’ve heard—consider sharing it. Accurate information is one of the most powerful tools we have in healthcare.