Disclaimer:
This article is intended for educational and informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. The content provided is not intended to be used for medical decision-making. Always seek the advice of a qualified healthcare provider with any questions you may have regarding a medical condition or treatment. Never disregard professional medical advice or delay seeking care because of information you have read in this article.
Heart failure is one of those medical terms that immediately triggers fear. The name alone sounds final, dramatic, and irreversible. Many people hear it and assume it means the heart is about to stop—or already has. Others confuse it with a heart attack. Some quietly panic, while others ignore early symptoms because they don’t think something so serious could apply to them.
Here’s the reality: heart failure is serious, but it is not hopeless. It is also far more common—and more manageable—than most people realize.
This article breaks down what heart failure actually is, why it happens, how it’s diagnosed, what modern treatment looks like, and what daily life with heart failure can realistically involve. Whether you’re reading for yourself, a loved one, or simply to understand the condition better, the goal is clarity—not fear.
What Is Heart Failure—Really? (And What It Is Not)
Heart failure does not mean that the heart has stopped beating. It also does not automatically mean death is imminent.
Heart failure means the heart is not pumping blood as effectively as the body needs. This can happen in two main ways:
The heart muscle becomes weak and can’t pump strongly enough.
The heart muscle becomes stiff and can’t fill properly between beats.
Either way, organs and tissues don’t get the oxygen-rich blood they need, and fluid begins to back up in places it shouldn’t—most commonly the lungs, legs, and abdomen.
Heart Failure vs. Heart Attack
This confusion is incredibly common.
A heart attack is a sudden event caused by a blocked blood vessel that damages part of the heart muscle.
Heart failure is a chronic condition that develops over time. A heart attack can lead to heart failure, but they are not the same thing.
A useful way to think about it:
A heart attack is a plumbing problem
Heart failure is a pump performance problem
Understanding this difference alone helps reduce a lot of unnecessary fear.
Why Heart Failure Is So Common Today
Heart failure is one of the fastest-growing cardiovascular conditions worldwide. This isn’t because hearts are suddenly weaker than before—it’s because medicine has changed.
Several factors explain the rise:
People are living longer
Aging increases the risk of heart disease, high blood pressure, and structural changes in the heart.Survival after heart attacks has improved
More people survive heart attacks today, which is a major success of modern medicine. However, damaged heart muscle can later contribute to heart failure.Chronic conditions are more common
High blood pressure, diabetes, obesity, and kidney disease place long-term strain on the heart.Better detection and diagnosis
Heart failure is being identified earlier and more accurately than in the past.
According to the Centers for Disease Control and Prevention, millions of adults in the United States are currently living with heart failure, and the number continues to rise each year.
The Different Types of Heart Failure (Without the Jargon Overload)
Heart failure isn’t one single condition. Understanding the type helps explain symptoms, treatment, and expectations.
Heart Failure Based on Ejection Fraction
Ejection fraction (EF) refers to the percentage of blood the left ventricle pumps out with each heartbeat.
Heart Failure with Reduced Ejection Fraction (HFrEF)
The heart’s pumping ability is weakened.Heart Failure with Preserved Ejection Fraction (HFpEF)
The heart pumps normally but is stiff and doesn’t fill well.Heart Failure with Mildly Reduced or Improved EF
These categories recognize patients whose heart function falls between ranges or improves with treatment.
This distinction matters because treatment approaches and outcomes can differ significantly.
Left-Sided vs. Right-Sided Heart Failure
Left-sided heart failure commonly leads to fluid backing up into the lungs, causing shortness of breath.
Right-sided heart failure commonly leads to fluid backing up in the body often causes swelling in the legs, ankles, and abdomen.
Many people have features of both.
Symptoms of Heart Failure: The Early Signs People Miss
Heart failure symptoms often start subtly. People frequently dismiss them as aging, stress, or being “out of shape.”
Common symptoms include:
Shortness of breath with activity or when lying flat
Fatigue and low energy
Swelling in the legs, ankles, or feet
Rapid or irregular heartbeat
Sudden weight gain from fluid retention
Waking up at night feeling short of breath
Needing extra pillows to sleep comfortably
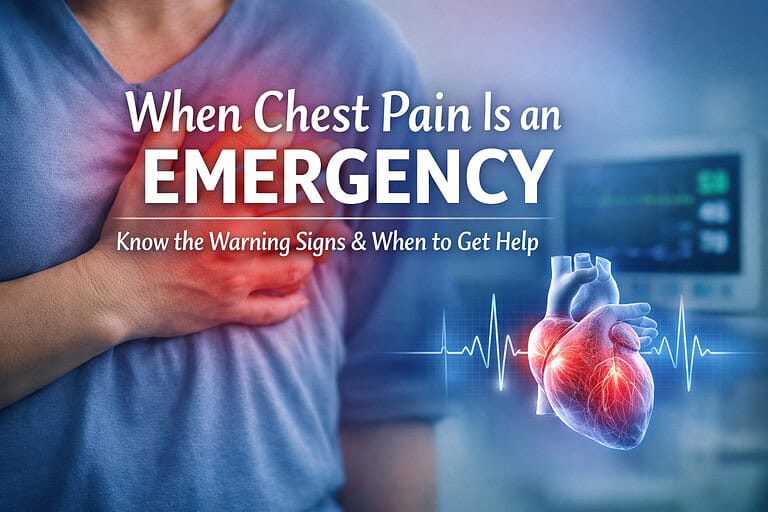
Warning Signs That Shouldn’t Be Ignored
Shortness of breath at rest
Chest pain
Confusion or dizziness
Pink, frothy sputum
Rapid weight gain over a few days
These symptoms may indicate worsening heart failure and require prompt medical attention.
What Causes Heart Failure?
Heart failure is rarely caused by one single event. It’s usually the result of years of strain on the heart.
Common causes include:
High blood pressure
Coronary artery disease
Previous heart attack
Diabetes
Obesity
Heart valve disease
Cardiomyopathies (genetic, viral, alcohol-related, or medication-related)
Think of heart failure as the heart’s response to long-term overload. When the heart is forced to work harder for years, structural and functional changes eventually occur.
Stages and Severity: How Doctors Classify Heart Failure
Clinicians use two systems to describe heart failure. Each answers a different question.
Disease Stages (A–D)
These stages describe progression over time:
Stage A: At risk but no structural disease
Stage B: Structural heart disease but no symptoms
Stage C: Structural disease with symptoms
Stage D: Advanced heart failure
Functional Classes (I–IV)
These describe how symptoms affect daily life:
Class I: No limitation
Class II: Symptoms with moderate activity
Class III: Symptoms with minimal activity
Class IV: Symptoms at rest
Someone can be Stage C but Class II—meaning they have heart failure but still function relatively well.
How Heart Failure Is Diagnosed
Diagnosis involves a combination of clinical evaluation and testing.
Common components include:
Detailed medical history and physical exam
Echocardiogram to assess heart structure and function
Blood tests that measure cardiac stress markers
Electrocardiogram (ECG)
Chest imaging
Lab work to evaluate kidney function and electrolytes
Diagnosis is not based on a single test but on the full clinical picture.
Modern Heart Failure Treatment: What’s Changed in Recent Years
Heart failure treatment has advanced dramatically. The goal today is not just symptom control—but longer life and better quality of life.
Core Treatment Goals
Reduce symptoms
Prevent hospitalizations
Slow disease progression
Improve survival
Medications
Modern therapy often involves multiple medication classes that work together to:
Reduce fluid buildup
Lower heart workload
Improve heart muscle function
Protect organs
Recent years have introduced medications that benefit patients across different heart failure types, including those with preserved ejection fraction—something that was not possible before.
Lifestyle and Self-Management
Medication works best when paired with:
Sodium awareness
Fluid monitoring
Daily weight tracking
Physical activity as tolerated
Regular follow-up care
Education and consistency are critical.
Hospitalizations, Readmissions, and Why Follow-Up Matters
Heart failure is one of the most common reasons for hospitalization among adults over 65.
The period immediately after discharge is particularly risky. Medication adjustments, symptom monitoring, and early follow-up visits significantly reduce complications and readmissions.
This is why clinicians emphasize:
Follow-up appointments within weeks
Clear discharge instructions
Patient and caregiver education
Heart failure care doesn’t end at the hospital door—it begins there.
Living With Heart Failure: What Daily Life Can Look Like
Living with heart failure looks different for everyone.
Many people continue to:
Work
Travel
Exercise
Enjoy social activities
Others may need to adjust expectations, pace themselves, or rely more on support.
Emotional and Mental Health
Heart failure can affect mood, confidence, and independence. Anxiety and depression are common and deserve attention just like physical symptoms.
Support systems—including caregivers, support groups, and healthcare teams—play a major role in long-term success.
The American Heart Association emphasizes patient education and self-management as key pillars of heart failure care.
Can Heart Failure Be Prevented—or Slowed?
In many cases, yes.
Prevention and slowing progression focus on:
Controlling blood pressure
Managing diabetes
Maintaining a healthy weight
Treating heart disease early
Avoiding smoking
Staying physically active
Even after diagnosis, early and consistent treatment can dramatically change outcomes.
Conclusion: What Heart Failure Really Means Going Forward
Heart failure is not a death sentence. It is a complex, chronic condition that requires understanding, management, and partnership with healthcare professionals.
Modern medicine has transformed heart failure from a rapidly fatal condition into one that many people live with for years—sometimes decades—with good quality of life.
Awareness matters. Early recognition matters. Education matters.
If you or someone you love has symptoms, risk factors, or a diagnosis of heart failure, the most powerful step is starting the conversation—asking questions, learning the signs, and staying engaged in care.
Understanding heart failure doesn’t remove its seriousness—but it replaces fear with clarity, and uncertainty with action.